Radiopharmaceuticals, which combine radioactive isotopes with biomarker identifying molecules, are at the forefront of precision diagnostics and targeted therapy in nuclear medicine. The manufacture of radiopharmaceuticals is a complex process due to radiation emitting isotopes and tight time constraints when the half-life of a radioisotope is short. This article briefly describes how a typical radiopharmaceutical drug product, a vial with an injectable solution, is manufactured.
The manufacture involves several key steps. As an example, manufacture of an F18 containing radiotracer is described (half-life ~ 110 minutes):
- Radioisotope production: Fluorine-18 (F18) entity is produced in a cyclotron from the reaction of high energy protons with O18 labeled water (H2O18). (The cyclotron is housed in the manufacturing facility.)
- Manufacture of a biomarker specific ligand e.g. manufacture of PSA (prostate Specific Antigen) identifying ligand for prostate cancer radioimaging or radiotherapy. The ligand is manufactured typically in a multi-step synthesis in an independent manufacturing facility and is a key raw material in the synthesis of a radiopharmaceutical.
- Radiolabeling reaction: Reaction of F18 entity with PSA identifying ligand to form a F18 containing radioligand. This reaction produces Active Pharmaceutical Ingredient (API) required for the drug product.
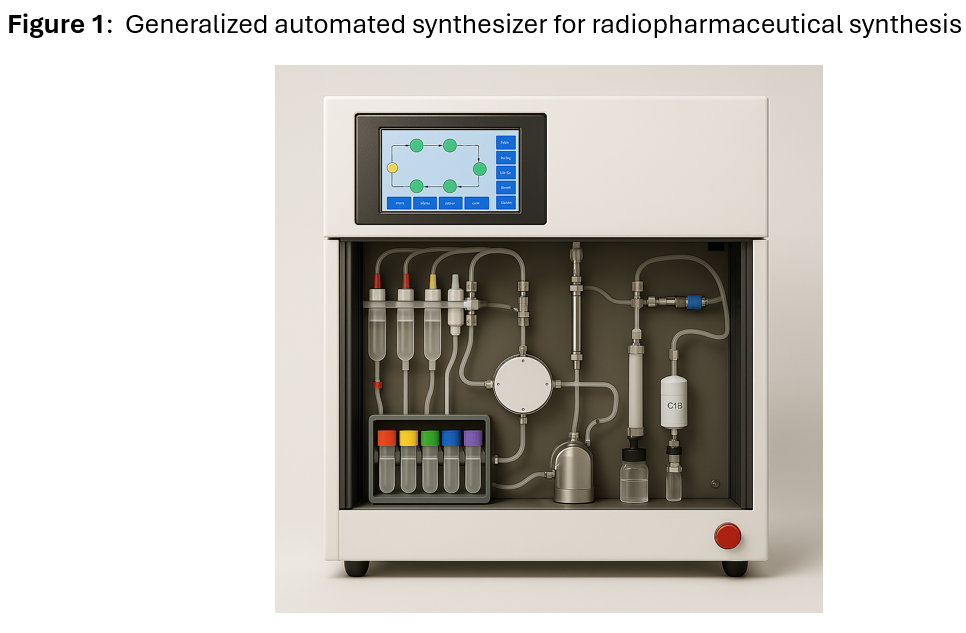
- Steps c-f are carried out in an automated synthesizer enclosed in a radiation protected glove boxes (hot cells) to contain the radiation. The operations are performed following GMP regulations under aseptic or sterile conditions. The hot cell is sterilized prior to operation and is located inside a clean room.
- Purification of radioligand (API), typically performed by HPLC.
- Formulation of API to sterile drug product: The API is formulated into a sterile drug product solution or suspension suitable for IV injection.
- Dispensing: Drug product formulation is dispensed into vials; vials are filled to specific volume based on dosage requirements. Vials are then labeled.
- Quality Control Testing. The drug product vials are tested for the following (not a comprehensive list but major quality control tests are covered): Radioactivity Measurement ( to ensure correct dose is formulated), Radioistope identity and purity ( to confirm radioisotope identity and to ensure radioisotopic impurities are within drug product specification), chemical purity (to ensure chemical impurities are within drug product specification), Sterility Testing (to ensure drug product is within specification for viable microorganisms), Bacterial Endotoxins (to control endotoxins that can cause adverse reactions in humans including fever).
It is crucial that drug product vials are transported in a timely fashion to end users (e.g. hospitals, imaging centers). A simplistic representation of an automated synthesizer is provided in Figure 1 below:
Overall, the manufacturing process of a radiopharmaceutical is highly specialized, complex and capital intensive. Handling radioactive materials requires specialized equipment, such as hot cells and facilities for storage of radioactive materials and disposal of radioactive waste.
Radiopharmaceuticals with short half-life radioisotopes can’t be stored long due to high rate of decay, which reduces their effectiveness for imaging or therapy with the passage of time. Centralized manufacturing therefore isn’t feasible for such radiopharmaceuticals. To cut down on transport time, production facilities are located near hospitals or imaging centers. Consequently, multiple manufacturing facilities are required to be qualified for manufacture for distribution of drug products over expansive geographical regions.
For a radiopharmaceutical containing a relatively long half-life radioisotope like Lu177 (half-life 6.6 days), centralized manufacturing and distribution is feasible.